In This Chapter
- Skimming the surface: Skin problems
- Avoiding (or stopping) worm infestations
- Reading your Pom’s body language for specific problems
- Knowing your Pom’s chances for hereditary challenges
Living with a pet for many years means dealing with illness — both minor and more serious, short-term and long-term. Unfortunately, because their life spans are so much shorter than ours, dogs tend to rush through the stages of life, rushing also into these illnesses at an advanced pace. But here’s the good news: When you’re able to extend their lives by even a short time in people terms, you’re actually extending it a long time for them.
In this chapter I show you how to recognize problems and address many of them on your own. I also point out when to turn a problem over to the veterinarian so you can extend your dog’s life and quality of life with the best care possible.
Saving Your Dog’s Skin
The best coat-care in the world can’t overcome skin problems. Itchy skin or skin that’s inflamed, greasy, or smelly, as well as skin with sores can all make your dog uncomfortable and her hair look lousy. Knowing a bit about different skin-related issues can help you identify and solve your dog’s skin problem.
Debugging your dog
Many people think a toy dog’s only job historically was to sit in people’s laps and look cute. But that concept’s only half right. Many toy breeds actually had a very important job — they were to sit in people’s laps, look cute, and attract fleas off the people.
Chances are you didn’t add a Pomeranian to your household for this reason. In fact, the roles have completely reversed and expanded: Now you’re getting fleas, ticks, and mites off your dog!
Making fleas flee
Fleas are little brownish bugs that scurry under your dog’s coat next to the skin. They can move pretty fast after you part the fur because they’re flattened and very narrow. They also leave behind poop that looks like black dirt and turns red if you get it wet. Fleas make your dog itch, both when they bite and afterward, because their saliva often causes allergic widespread reactions for days afterward. They also transmit tapeworms. After they get into a home or environment, fleas hang around, sometimes for months, waiting for a warm, fuzzy host to stroll by.
Fighting fleas — the scourge of dogdom — had been a losing battle until recently. Not so long ago you had to soak your dog, your house, and your yard in so many poisons that it made Chernobyl seem like a nature preserve. The time and expense added up until some owners finally gave up.
Today the situation’s improved. Newer products available from your veterinarian have a higher initial purchase price but are cheaper in the long run because they work from the get-go and need reapplication only once a month or so.
Most of these products are available only from your veterinarian, although some discount products try to sound like they’re just as effective. Look for a product with one of the following ingredients:
– Nitenpyram: If your Pom is covered in fleas, reach for this oral medication that has the fleas kicking the bucket within two minutes. Every flea is dead within four hours. The drawback? Nitenpyram has almost no residual activity, so it’s mostly a quick fix for heavily infested dogs.
– Selamectin: Want something that does it all? This chemical takes care of fleas, ear mites, and several internal parasites for one month and acts as a heartworm preventive. But if your dog doesn’t need all this, don’t go overboard. Opt for just what he does need.
– Imidacloprid: Only bothered by fleas? Apply this spot-on chemical between your Pom’s shoulder blades. It distributes itself all over the dog’s body within a day and kills fleas for a month. Your dog can get wet, but repeated baths will wash the product off.
– Fipronil: Are ticks also a concern? This chemical collects in the hair follicles and wicks out over time. It kills fleas for up to three months and ticks for a shorter time, and it’s resistant to bathing. It’s sold as a spray or as a spot-on, a liquid applied to the back.
– Permethrin: If fleas aren’t a big problem for your dog (for example, you’re on a trip and just found one or two fleas), this short-term, very safe spray may be your answer. But don’t rely on it for anything more than a quick fix.
– Lufenuron, methoprene, or fenoxycarb: Have a flea problem that’s spread to the house or yard? These chemicals render fleas sterile. It doesn’t kill them though, so you’ll need something else for that. You can also spray your home and yard with poisons, but sterilizing the fleas is generally safer for you and your dog.
Tip
Your best bet? Use a combination of products. Fleas are building up immunity to some of these chemicals. By alternating between two or more of them with every application, you catch the few fleas that were immune to the previous chemical. And don’t scrimp on products! Use them frequently enough (once a month, in general) and heavily enough to make sure there are no survivors!
The later section “Alleviating allergies” contains additional information about fleas with regards to your dog’s allergic reaction to them.
Getting ticks unstuck
Ticks are fairly small parasites — some are smaller than the head of a match, some a bit larger, especially once they’re puffed up with your dog’s blood. They live off the blood of mammals, and they can stick to your dog’s skin for long periods of time if you don’t get them off. They’re harder to kill than fleas, but at least they hold still.
The most common way to get rid of ticks on your dog is to remove them one by one. Feel all over your Pom’s body, but especially around the ears, neck, and between the toes for the telltale bumps. Then use a tissue to grasp the tick as close to the dog’s skin as possible, and pull it gently out — don’t jerk it. Even if you leave part of it, it won’t hurt your dog.
Tip
Another way to kill ticks is with chemicals. Products containing amitraz (usually found in tick collars) or fipronil (usually found in sprays or spot-on applications) kill ticks. However, they don’t kill the ticks immediately, so chemicals are typically reserved as backups. Your hands are still your best tool.
Warning!
Ticks are a particularly serious concern because they can transmit several diseases such as Lyme disease, erhlichiosis, Rocky Mountain spotted fever, and babesiosis. A vaccination is available for Lyme disease, but it’s not advisable for dogs that don’t live in Lyme endemic areas. Your veterinarian can order blood tests if any of these conditions are suspected — for example, if you live in an area where one of these diseases is common, if your dog is suddenly lethargic, or if he has intermittent lameness.
Taking the bite out of mites
Mites are tiny bloodsuckers that can make your dog’s hair fall out. I detail the three different types of animal mites in Table 11-1.
Alleviating allergies
When people have allergies, they tend to sneeze. But when dogs have allergies, they tend to itch. The most common allergens for dogs are flea saliva, pollens, dust mites, and food. A veterinary dermatology specialist can perform intradermal (skin) testing with common allergens but not food allergens. If the culprit is identified, a series of injections can often help the dog overcome the allergic reaction. A good clue: If your dog is biting at her skin, especially her front feet, scratching at her ears, or rubbing her rump on your furniture frequently, take her to the vet to see whether something else could be the cause and to get temporary relief.
Flea allergies
Flea allergy dermatitis, or FAD, is the most common of all skin problems. With FAD, a dog is allergic to flea saliva, so not only does the dog suffer from the normal itchiness due to these small critters walking around on his skin, but he also suffers because the saliva acts as a skin irritant. So the poor pooch reacts the only way he can — by biting or chewing at his skin to make the irritation stop.
In a flea-allergic dog, the saliva from just one flea bite can send the dog chewing not just around the bite but all over, especially on the rump, legs, and paws. And this chewing often leads to crusted bumps in these areas. The solution is simple: Get rid of every flea! (See the section “Debugging your dog” earlier in this chapter.)
Airborne allergies
Inhaled allergens are similar to those that affect humans — pollen, dust mites, and molds. Your dog may have a skin allergy if you see him frequently scratching or chewing at his face, ears, feet, forelegs, armpits, and abdomen. Because the feet are so often affected, many people assume the problem is grass or carpet allergies, but that’s seldom the case. It’s just that allergies from anything anywhere tend to make the feet itchy.
Table 11-1 | Animal Mites to Watch Out For |
Type | Disease | Symptoms | Treatment | Notes |
Cheyletiella mites | Walking dandruff | Mild itching and dandruff especially along the back; mites move under the dandruff scales, so dandruff appears to move | Repeated antiparasitic shampoos, or dips in amitraz, or high-dosage heartworm preventive drugs such as ivermectin | Contagious; every dog in a household needs treatment; spread by direct contact and bedding; some breeds, including Poms, are more prone |
Demodex mites | Demodectic mange | Hairless spots, most often on the face, feet, and front legs; may be red but are not itchy | Repeated dips in amitraz or high-dosage heartworm preventive drugs such as ivermectin | Noncontagious but often difficult to treat; a few small patches in a puppy usually go away, but many patches or a generalized condition require treatment |
Sarcoptic mites | Sarcoptic mange | Intensely itchy small bumpsand crusts on the ear tips, abdomen, elbows, and hocks | Repeated dips in amitraz or high-dosage heartworm preventive drugs such as ivermectin | Extremely contagious, even to people; all animals in household should be treated |
Common short-term treatments include allergy pills or steroid medication. Bathing in cool bath water with anti-itch shampoos from your veterinarian may help. Long-term treatments including moving to another state or getting allergy tests and injections. Moving may be the less expensive option.
Food allergies
Food allergies can produce diarrhea or itchy skin and ears. Your veterinarian can prescribe an elimination diet (a diet consisting of novel proteins your dog hasn’t eaten before, such as those from venison, duck, or rabbit). No, you don’t have to get out the gun. These proteins are available in dry and canned foods from your veterinarian. You keep the dog on the diet for at least a month, withholding treats or anything else that may contain a food allergen.
If the dog’s symptoms clear up, then you can add back ingredients he has been exposed to one at a time. If and when you see a return of the allergy symptoms, you know which one causes the problem. You may have to keep your dog on a special diet for the rest of his life.
If his condition doesn’t clear up, he may need to try another novel diet or a hypoallergenic diet that has a special protein molecule size. Some dogs’ food allergies never clear up, though.
Cooling hot spots
Hot spots, more technically known as pyotraumatic dermatitis, are red, itchy, painful, moist spots that seem to arise overnight. Usually something has irritated the skin, perhaps a flea bite, and the dog scratches and chews the spot. The skin gets irritated and moist, allowing first infection and then worse symptoms to set in.
If your Pom has hot spots, clip the hair away, prevent the dog from chewing or scratching, and apply a treatment that both dries the skin and kills the bacteria. (For the best results, use antibiotic powder, which you can get over the counter for people, or even bacteria-fighting mouthwash on the skin.) You may also need to give your dog an oral antihistamine to stop the itching, or your vet can prescribe steroids. (See the sidebar “Easing the itch” for more ideas.)
Easing the itchIf your Pom is itching to scratch for any reason, you can ease the itch at home with several treatments. Here are a few: – Apply an ice pack or even immerse the dog in cool water. Pat dry, but avoid blow-drying or vigorous rubbing.
– Bathe with medicated shampoo and cool water, leaving the shampoo in contact with the skin for at least ten minutes; then rinse and dry thoroughly.
– Pour a little aloe vera juice on the irritated area and leave it on.
– Apply a topical nonitch spray, witch hazel, moisturizing spray, or topical steroid medication sold for humans.
– Try to get your dog’s mind off the itch. Play some games, go for a walk, or give a treat that requires extensive chewing or working.
– Fatty acid supplementation (fish oil, which you can buy in any drug store, is one good source) can provide improvement over the long term. It’s effective in up to one fourth of the cases of itchy skin, especially when used with antihistamines.
Note: Don’t confuse these supplements with those sold as food supplements to improve coat quality.
– Your veterinarian can suggest a safe dose of antihistamines. Common human antihistamines safe for dogs are clemastine fumarate, diphenhydramine, chlorpheniramine, and hydroxyzine.
Histamines don’t cause as much inflammation in dogs as they do in humans, so antihistamines may not be as effective in dogs. Finding the most effective types usually takes a couple of weeks of trying each one out.
Antihistamines may cause drowsiness, a desirable side effect in cases of intense itching but not great for long-term use.
Don’t give your dog any over-the-counter antihistamines that contain other medications, such as those in sinus or cold-relief medications. Talk to your veterinarian ahead of time to find out the correct dosage for your puppy and keep some in the medicine chest.
If itching continues, your veterinarian may prescribe short-term oral cortisone medication. This treatment provides the most immediate and effective relief and may be necessary in order to start treating the itch. |
Global Deworming
If you see small, flat, white segments in your dog’s stool, she may have tapeworms. Because she gets them from eating a flea, the best prevention is flea prevention (see Chapter
Maintaining Your Pom’s Health and Happiness). Tapeworms may gross you out and make your dog’s butt itch, but as worms go, they’re not terribly devastating. Still, you need to get rid of them. Tapeworms require special deworming medication, but you don’t need to rush to the vet. Just describe what they look like to the receptionist, or if you’re not sure what they are, bring one in for verification, and your vet will usually hand you some pills. Get rid of the fleas too while you’re at it.
Warning!
You may be tempted to pick up some over-the-counter deworming medicine at the grocery store and just blast those worms away every month. Don’t! These dewormers are neither as effective nor as safe as those you can get from your veterinarian. By performing a fecal check, your veterinarian can provide the best medicine for the specific parasite.
Spotting Signs of Sickness
If only your Pom could tell you where it hurts — or whether it hurts. Few challenges are as frustrating as determining whether your dog’s sick, and if so, what the problem is. But when you know what to look for, you discover your Pom’s telling you more than you ever imagined.
Butt scooting
Your Pom may look comical doing the butt-scootin’ boogie, but it’s no laughing matter for her. She’s trying to make her sore butt feel better by relieving some of the pressure in her anal sacs, the two sacs just inside and on either side of her anus.
Technical Stuff
The sacs normally contain a sticky fluid that squeezes out when the dog defecates or occasionally squirts out, skunk-like, if she’s suddenly alarmed. If the tiny holes in the sacs get clogged, the fluid builds up, thickens, and expands the sacs balloon-like until they push through the skin to the outside and then burst. To add to the problems, the sacs become inflamed and infected. Talk about a bad-feeling butt!
Besides scooting, your Pom may constantly lick at her anus in an attempt to soothe it. Your veterinarian can unclog the sac and express the fluid as a routine matter so your Pom feels better almost immediately.
Remember
Two additional problems may cause scooting:
– Tapeworms wriggling around the anus. (See the previous section “Global Deworming” for the remedy.)
– Lower-back problems. If the anal sacs are okay and no tapeworms are present, have your veterinarian check your Pom’s spine.
Coughing
Everybody coughs once in a while. But if your Pom’s coughing every day or in long bouts, that’s not normal. Your veterinarian can do some simple tests to pinpoint the problem.
Especially in younger dogs, coughing may indicate an infectious disease. Kennel cough is a group of highly contagious airborne diseases caused by several different agents, but most often by Bordetella, a type of bacteria. Kennel cough is characterized by a gagging cough that starts about a week after exposure.
Tip
Your veterinarian can inoculate your Pom against kennel cough, usually with nose drops, but protection doesn’t last more than a few months and may not cover every possible infectious agent. Nonetheless, the inoculation is a good idea if you plan to board your dog or if he suffers from tracheal collapse or other breathing problems. (See the later section “Pondering Pom Predispositions” for more on tracheal collapse.)
Coughing can also be a sign of congestive heart failure, tracheal collapse, or even lung cancer. Because these are life-threatening conditions, your veterinarian should check out any coughing that persists more than a couple of days.
Diarrhea
Your little squirt can get a case of the squirts for lots of reasons: Nerves or a change in food or water can cause short-term problems; intestinal parasites, sensitivity to certain foods, and illnesses can cause more long-lasting diarrhea.
A little bit of blood in diarrhea is not the cause for concern in dogs that it is in humans. Intestinal parasites such as
giardia or
coccidia (see Chapter
Maintaining Your Pom’s Health and Happiness) can cause blood in the stool. Nonetheless, if it continues for more than a day, or if it’s in copious amounts, you need a veterinarian’s opinion. A Pomeranian has so few reserves that a bout of diarrhea can seriously dehydrate her. She may need to go to the veterinarian for intravenous fluids.
Tip
Take these steps to stop diarrhea:
1. Restrict food for a meal or two, feeding just a partial meal.
2. Offer a bland diet consisting of rice (or tapioca or cooked macaroni) along with tofu (or nonfatty chicken) for several days when you start to feed her again.
You want to give the intestinal tract time to heal, and it can’t do that with fatty food encouraging more diarrhea.
Ear gunk
Pomeranians are blessed with healthy ears in part due to their prick-ear design that lets air circulate within them. Nonetheless, like all dogs, their ear canal has an initial vertical segment that abruptly turns inward at a sharp angle. That sharp angle can restrict some air flow, which encourages moisture, which in turn nurtures bacteria and yeast. Although certain types of bacteria are normal and harmless in the ear canal, others can grow unchecked, causing the ear canal’s surface to react to their byproducts by secreting oils and becoming inflamed.
Other factors contribute to ear problems:
– Allergies are the most common cause of ear problems in dogs overall. See the section “Alleviating allergies” to determine if this might be the problem, and what you can do to stop the itch.
– Seborrhea causes itchiness and contributes to a heavy accumulation of ear wax. Other parts of the dog may have greasy skin and hair. Your vet may be able to diagnose and treat this.
– Parasites, such as ear mites, can also cause intense itching of the ears. Your veterinarian can diagnose the presence of parasites easily and can prescribe much more effective medication for ear mites than you can buy over the counter.
Signs of ear problems can include
– Head shaking
– Head tilt
– Scratching at the ear
– Rubbing the ear
– Smelly ear
– Dark buildup within the ear
Warning!
A veterinarian should examine all ear problems for the following reasons:
– The same symptoms can result from various causes that require different treatments.
– A perforated ear drum due to chronic problems requires medication that’s different from the medication for an intact ear.
– If the ear is filled with wax and debris, it needs to be cleaned so that antibiotic medication can reach the lining of the canal. But if the ear is painful or the ear drum is perforated, the dog must be sedated to clean the ear.
In most cases the veterinarian sends you home with an ear flush solution in addition to antibiotic medication. The solution loosens wax and debris (so the medication can reach the ear’s surface) and has a drying agent so it doesn’t leave the ear wet — find out how to use it in Chapter
Primping Your Pom. To apply the medication, first clean the ear with the solution, and then squeeze the medicated ointment or drops into the canal, again gently massaging the base of the ear to disperse the medicine.
Tears and eye goop
No doubt you look at those pretty Pom peepers more than any other part of your dog. So while you’re at it, keep an eye out for eye problems such as squinting, tearing, or mucous discharge. These signs can indicate lid problems, foreign bodies, tear drainage problems, or dry eyes.
Watery tearing is the least worrisome eye problem. Dogs frequently have blocked tear ducts that cause tears that normally drain from the eye socket to overflow onto the cheek. Your veterinarian can do a simple test to see whether the duct’s blocked, and in some cases she can flush it out.
But the duct in many toy dogs is simply too small and your pup may just have to live with it. You can combat the staining below her eyes by wiping the tears often with an over-the-counter eye wipe specifically for tear staining. Turn to Chapter
Primping Your Pom for additional solutions.
If the tearing is chronic, if the eye shows any other signs of discomfort, or if the discharge is thick rather than watery, then a veterinarian needs to check your dog. Your Pom may have
– An infection, which can be treated with antibiotic drops.
– An irritation to his cornea, which may also be treatable, or a lid problem that needs attention.
– Dry eye syndrome, or keratoconjunctivitis sicca (KCS). The dog doesn’t produce a normal amount of tears, so the cornea (the outer clear coat of the eye) dries out and looks dull. The eye may have a thick discharge, and the dog may blink, squint, and rub at his eyes. Your veterinarian can diagnose the condition with a simple tear test and prescribe several treatment options.
Limping
Your Pom may not be expected to run the Iditarod, but he does need to run around your house on all four legs. All dogs can stub a toe and end up a little gimpy now and then. But if your dog is favoring one leg and not using it, examine the leg for broken bones, tenderly feeling down the leg’s length and comparing every bone, including those of the foot, with that of the leg on the other side. A broken bone, of course, needs veterinary attention.
You can treat less serious injuries at home. Follow these suggestions:
– Ice packs help minimize swelling if applied immediately after an injury, but moist heat is better for older injuries.
– Complete rest, even if it means locking your Pom in a crate, is the best medicine for most cases of lameness. Rest him well past the time he appears to be cured.
– Let him resume exercise gradually and on a leash.
– If three days go by with no improvement, you need to get a veterinary opinion.
Aside from injury, an all too common cause of rear-leg lameness is patellar luxation (see the later section “Pondering Pom Predispositions” for more on this problem) or sometimes, Legg-Calve-Perthes (destruction of the head of the femur [thigh] bone that may start at 3 to 4 months of age. Treatment is absolute rest or surgery to remove the femur head.) Neither is an emergency, but the sooner your veterinarian diagnoses them the better because they only get worse with time.
Listlessness
When your Pomeranian pistol suddenly prefers to stay in bed rather than play, take time to study her. Is she bored, tired, or really sick? Poms can be misleading because they can push aside their feelings of malaise and show up waggy-tailed for a favorite activity such as a walk or ride if you tempt them enough. Of course, dogs gradually slow down as they mature and age, but a relatively sudden change in activity level is cause for a trip to the veterinarian. Look for these clues:
– A sick dog often lies in a curled or hunched up position rather than sprawled out. This is a go-to-vet-today situation.
– A dog with a high fever is usually lethargic. Take the temperature (see Chapter Maintaining Your Pom’s Health and Happiness), call the vet if it’s over 103 degrees, and go to the emergency vet if it’s over 105. Cool the dog with wet towels in either case.
– A dog with anemia or circulatory problems may seem weak. Call the vet right away if the gums are white or gray.
– A dog having a hypoglycemic episode (low blood sugar; see Chapter Eating Out of the Pom of Your Hand) may sleep (even when you try to rouse her) or stagger and appear uncoordinated. Rub corn syrup on the gums and go to the emergency vet right away.
– An uncomfortable dog may walk around restlessly, dig at the ground, lie down, and then get right back up. This dog needs to see the vet as soon as possible.
– A dog with abdominal pain often stands with her rear in the air and the front flat to the ground, as though stretching. If this continues more than an hour, see the vet promptly.
– A dog having a hard time breathing is often reluctant to lie down; if she does, she lies on her stomach with head up and nose pointed upward. This is an emergency vet situation.
– A dog in pain may shiver, pant, or both. See the vet right away if it continues.
Loss of appetite
If your Pomeranian sticks his pointy nose up at dinner occasionally, don’t think it’s cause to rush to the veterinarian. But if he’s been a hearty eater and then gradually leaves more and more in his bowl, he needs to be checked out. By the same token, if he suddenly stops eating and misses more than a meal or two, something’s probably not right. Take into consideration, though, that dogs eat less during hot weather.
Warning!
Because of the dangers of hypoglycemia (see Chapter Eating Out of the Pom of Your Hand), you’re wiser to overreact than to wait and see, especially with tiny, thin, young, or older Poms.
A spoonful of sugar or blatant trickery: Giving your Pom medicineMedicine that sits in the bottle or splatters all over the floor doesn’t do your Pom (or your wallet) much good. But managing to get pills and liquid medicine where they need to go can be frustrating if not downright impossible. For pills, try one of these options: – The stick-it-down-the-throat option: Gently open the mouth, place the pill as far back as possible (aided by a tiny shove with your index finger), close the mouth, and gently rub the throat. You also can buy a piller, a small plunger that takes the place of your finger. If your pup is used to you opening her mouth and handing her a treat from puppyhood, this should be a snap.
– The hide-it-in-food option: Unless medical reasons prevent this method, hide the pill in a bit of peanut butter or liverwurst. If your Pom’s suspicious and filterfeeds her way through the food, add these steps:
- Make three balls of food.
- Feed her the first one to convince her that the food’s safe to eat.
- Feed her the second one that holds the pill.
- Excitedly show her the third ball before she finishes the second one so she wants to eat the second one, plus pill, in a hurry.
- Give her the third ball.
Liquid medicine is tougher to administer than pills. You need to pull out one cheek so it makes a little pocket, squirt the stuff in, and hope for the best. (And giving a little treat as a reward never hurts.) |
Urination changes
You may notice that your dog has accidents or needs to go out more often than normal. This clue means you need to pay close attention to her. Several disorders can cause changes in urination, and the types of changes vary widely. Your veterinarian can often pinpoint the problem with a simple urinalysis.
– Urinating small amounts suddenly and often, especially in females, may indicate a urinary tract infection. The dog may also cry out when urinating. Antibiotics can cure this uncomfortable condition, and cranberry tablets can help prevent this condition in Poms that are prone to it.
– Dribbling urine during sleep most commonly occurs in spayed females. Drugs often treat it successfully.
– Cloudy or bloody urine can indicate infection of the prostate or bladder. The dog may also strain to urinate. These infections can be extremely painful and require antibiotic treatment. Left untreated, they can reach the kidneys and cause even more serious problems. Castration is usually the treatment of choice for males with repeated prostate problems.
– Painful urination, often with blood in the urine, can indicate urinary stones, especially in males. These stones can be diagnosed with a radiograph and often controlled with diet. Surgery may be necessary initially to resolve the problem, however.
– Increased urination and increased thirst can indicate diabetes or kidney disease. Diabetes can be diagnosed with a urine test and controlled through diet and insulin injections. I cover ailments common in older dogs, including kidney disease, in Chapter Maintaining Your Pom’s Health and Happiness.
Warning!
– Inability to urinate is an condition that requires immediate veterinary attention.
Vomiting
Every dog owner has been awakened by the “urp, urp, urp” of precious Patty puking all over the best carpet in the house. Dogs seem to vomit almost as a recreational activity.
Remember
Vomiting is a concern when it
– Continues for more than three upheavals at a time
– Contains more than a tiny bit of blood
– Contains a substance resembling coffee grounds (it’s partially digested blood)
– Contains anything resembling fecal material (unless your dog eats feces)
– Accompanies any other symptoms of illness such as lethargy or diarrhea
– Has no results (the dog repeatedly tries to vomit but nothing comes up)
All these instances merit a call to the veterinarian.
Tip
Sometimes dogs vomit early in the morning simply because their stomachs are empty. Feeding your dog a late-night snack can fix the problem. In another scenario, dogs often vomit after they eat grass. Nobody knows exactly why they do this, but it seldom means your dog is sick.
Two different breeds of medicineJust as with human medicine, complementary and alternative therapies may help your sick dog. Complementary therapies are out-of-mainstream veterinary medicines that accompany mainstream therapies; alternative therapies replace mainstream therapies. Many veterinaries use both traditional and nontraditional therapies in their practices. Popular complementary and alternative therapies include acupuncture, aromatherapy, Bach flower therapy (for emotional harmony), botanical medicine, chiropractic, homeopathy, magnetic therapy, massage therapy, nutraceutical (natural foods) therapy, nutritional therapy, and physical therapy. For more information, visit AltVetMed, the most comprehensive source for alternative veterinary medicine on the Web, at www.altvetmed.org. |
Pondering Pom Predispositions
Like all breeds, Pomeranians descend from a comparatively small group of founding fathers and mothers that were eventually interbred so that today’s Poms are all related to one another. So the entire population forms what geneticists call a closed breeding population. Unfortunately, every dog (Poms too) averages six deleterious (bad) recessive genes. As Pom descendents started to interbreed, chances naturally increased for both a father and a mother to carry the same bad genes. As a result, their progeny inherited two copies of that gene and inevitably exhibited the undesirable trait.
So every breed of dog has passed its own menu of hereditary headaches down through generations. Breeders try to avoid pairing parents who may carry the same recessives genes — and with the advent of DNA testing, that solution’s becoming more and more effective. But genetic problems are still a long way from disappearing. Meanwhile, be on the lookout for the Pomeranian predispositions covered in this section.
Alopecia X: Hair loss
Pomeranians have one hair trait that they’d rather do without: a condition called alopecia X. Common to many of the spitz breeds, the condition goes by several other names: black skin disease, castration responsive alopecia, and growth hormone responsive alopecia. Because the condition is much more common in males than females, researchers speculate that it’s gender-linked.
The trait seems to have two forms:
– Early onset form: A puppy grows a luxurious puppy coat, sheds it, and no adult coat ever replaces it.
– Late onset form: A Pom with a normal adult coat loses guard hairs, which leaves the fuzzy undercoat and gives the dog a puppy-coat look. Eventually the undercoat goes, too. The bald skin turns dark, but the dog doesn’t seem uncomfortable or itchy.
Because this hair loss occurs in several other disorders, your veterinarian will test your Pom’s blood, urine, and skin to rule out hypothyroidism, Cushing’s disease, and other conditions.
For some reason, spaying or castrating resolves the condition in many dogs, so that’s the first step if your Pom hasn’t been fixed. The dog often grows a full coat within months of the surgery, although the coat isn’t always permanent.
If neutering your dog doesn’t work, the next step is melatonin (hormone) tablets, which help 50 percent of dogs within three months. If the hair does grow, you can eventually taper the dosage, but he’ll probably need to stay on some dosage forever.
Ask your veterinarian about the pros and cons of other options such as therapy with adrenal sex hormones, methyltestosterone, lysodren, growth hormones, prednisone, and cimetidine, which have varying degrees of success. Some of these have undesirable side effects, so they aren’t generally first choices.
Remember
Alopecia X is mostly a cosmetic condition; at some point you may find it’s better to simply accept it than to administer drugs that adversely affect your Pom’s health. For more information, go to www.pcoc.net/black-skin-disease.htm.
Entropion: Eyelid problems
With entropion, an eyelid (usually the bottom one) rolls inward toward the eye. The lashes irritate the cornea, causing tearing, squinting, and perhaps sensitivity to light. If the cornea continues to be irritated, it can actually develop ulcers and scars that impair vision. Entropion is hereditary, although the exact genetic mechanism is unknown.
The condition is often first noted in puppyhood, but some pups outgrow the disorder as the face structure changes. For this reason, veterinarians don’t perform surgery on pups but may temporarily tack the lid to help alleviate any discomfort. If the lid still rolls inward after the dog’s matured, major surgery can resolve the problem. Because it’s better to undercorrect than overcorrect, more than one surgery may be necessary.
Help find a cureYou can help the future health of Pomeranians by contributing to health research, either with money or samples. For example, at the time of this writing, the Canine Health Foundation is sponsoring research into alopecia X in Pomeranians. Monetary contributions from individuals are needed to supplement the funding, however. In addition, researchers need blood samples from Pomeranians, both normal and affected, in order to find the gene or genes responsible. Go to www.pcoc.net/blackskin-disease.htm to find out how to contribute or participate. |
Hydrocephalus: Water on the brain
Small dogs with a tendency toward domed heads, such as Poms, seem to be predisposed to hydrocephalus, or water on the brain.
Technical Stuff
The brain is normally bathed in cerebrospinal fluid, which is constantly produced, circulated, and reabsorbed. In some dogs, either too much fluid is produced or too little is reabsorbed, so the fluid accumulates around the brain, pushing the soft bones of the puppy’s skull outward and giving the appearance of a big, round, head. After the skull hardens with maturity, it can’t expand, so the excess pressure pushes in on the brain.
A Pom puppy with hydrocephalus generally has the following symptoms:
– An abnormally round skull at 12 weeks old
– An open fontanel (soft spot)
– Eyes that diverge so that each is directed outward (the opposite of cross-eyed)
– Seizures or blindness
– Presses her head into walls
– Is extremely difficult to housetrain
Your veterinarian can take radiographs. A definite diagnosis usually requires more sophisticated scans from specialists.
Poms with mild hydrocephalus can live long and full lives, but may be somewhat mentally retarded. In most cases, though, the condition gradually worsens throughout puppyhood. Drugs can temporarily decrease pressure and swelling, but they’re not usually a lifelong fix.
Remember
For a more permanent fix (needed in all but the mildest cases), a specialist places a small tube in the brain to drain the excess fluid to another part of the body. The shunt must be replaced as the puppy grows, and complications often occur. Because of the difficulties treating hydrocephalus, euthanasia is often recommended.
Open fontanel: Soft spot
Just as with a human baby, a canine infant is born with the bony plates of the skull somewhat soft and separated. These bones usually harden and gradually fuse together over two to three months. In some Poms, the plates never fuse and a soft spot, the fontanel, remains throughout life.
Because the skull’s function is to protect the brain, obviously a soft spot is a worry. A hit on the head in just the wrong place can mean brain damage. Affected dogs don’t know they should be more careful, and most Poms with open fontanels are never bothered by them — except by their owners’ fretting. No treatment is available.
Patellar luxation: Bad knees
Have you seen a dog that takes a few steps, then holds one hind leg up and forward, skips a step or two, and then take a few more steps? At first this may look like a jaunty little jig, but more likely it’s a challenging condition called patellar luxation.
Technical Stuff
This common problem involves the patella (kneecap) of one or both rear legs. Normally, the patella slides up and down in a small groove of the femur (thigh bone) as the leg bends and the knee moves. But if the groove is too shallow or the tendon of the quadriceps muscle has too much rotational pull, the patella can ride over the side of the groove.
Because the luxated (out-of-place) muscle has to relax before the patella can pop back into place, the dog often hops for a few steps with the leg straight until the patella pops back. This popping hurts (your dog may yelp) and wears down the ridge, causing the condition to worsen.
In small dogs, signs of patellar luxation appear as early as 8 weeks of age but usually are apparent by 6 months; the patella tends to slip toward the inside, giving a bowlegged look. Early diagnosis is helpful in slowing the progress, but treatment depends on the severity of the condition. Table 11-2 presents the levels of patellar luxation.
Table 11-2 | The Four Grades of Patellar Luxation |
Grade | Characteristics | Patella Movement | Surgical Recommendation |
1 | Dog occasionally skips, keeping one hind leg up and straight for a step or two | Can be pushed out of position by hand but easily returns to correct position | Surgery may be unnecessary |
2 | Dog often holds affected leg up and straight when moving | May not slide back into position by itself | Surgery |
3 | Dog uses affected leg infrequently | Usually out of position; slips back out almost as soon as it’s replaced | Surgery |
4 | Dog never puts weight on the leg | Always out of position and can’t be replaced manually | Surgery |
Cases that appear in puppyhood usually develop into grade 3 or 4 in adulthood. Cases that first appear in young adults usually develop into grade 2 or 3. Cases that first appear in older adults are usually grade 1 or 2.
Surgery to tighten any stretched tissues and reconstruct the groove or realign the muscle can improve the condition. A young dog with grade 1 or 2, or any age dog with grade 3 or 4, is a candidate. Surgery may not make the leg perfect, but it will enable your Pom to run and walk relatively free of pain. An orthopedic specialist has the best chance of successfully treating the condition.
Tip
Glucosamine supplements may help to build cartilage and may be helpful for grade 1 cases, but they aren’t much help in more serious cases.
Remember
The Orthopedic Foundation for Animals maintains a registry for dogs that have been screened for patellar luxation. Although only a limited number have been evaluated, Pomeranians have the unfortunate distinction of having the highest percentage (48 percent) of the condition of any breed. Most veterinarians believe the condition is hereditary in Poms.
Patent ductus arteriosus: Heart defect
Patent ductus arteriosus (just call it PDA) occurs when a blood vessel (the ductus arteriosus) fails to close after birth. The function of this blood vessel is to bypass the nonfunctioning lungs during fetal life. So when it stays patent (open and working) after birth, the vessel sends blood that’s supposed to go to the rest of the body to the lungs instead.
Most puppies with PDA seem completely normal except for a heart murmur. Your veterinarian can hear the murmur, but a veterinary cardiologist usually makes an exact diagnosis. PDA can lead to heart failure. Although drugs can control the signs of heart failure, the best treatment is early surgery, preferably by 5 months of age (before permanent damage can occur). Without surgery, life expectancy is about two years. With surgery, the dog should be able to live a full life.
PDA is the most common hereditary heart problem in dogs, and it’s particularly prevalent in Pomeranians, especially females.
Tracheal collapse: Breathing problems
Tracheal collapse is most common in toy breeds. The trachea, or windpipe, consists of a series of cartilage rings. In some Poms, the cartilage isn’t as rigid as it should be, so some of the rings collapse, flattening the trachea and obstructing breathing. If the collapse is in the neck area, the dog has trouble inhaling. If the collapse is in the chest area, the dog has trouble exhaling.
Remember
Several factors (like obesity, respiratory infection, enlarged heart, endotracheal intubation, or inhalation of irritants or allergens) can make a tracheal collapse episode more likely. Coughing, which is a major symptom, can also make the condition worse.
Poms and anesthesiaAnesthesia, though not without risks, is far safer today than several years ago, when injectible barbiturate anesthesia was popular. Newer inhalant anesthesias (like isoflurane and sevofluran) and newer induction agents (like propofol) are far safer than traditional agents. Risks can also be reduced by a presurgical health check that includes blood testing and by careful monitoring during surgery. Because of a Pom’s tiny trachea, the veterinarian must be extremely careful when placing the tube. Your best veterinarian is one experienced with surgery on tiny dogs. |
Affected dogs often cough with a harsh, goose-like honk, especially when they’re excited, when pressure is put on the throat, or when they’re eating or drinking. In severe cases, the dog can’t get enough air, causing him to faint and get a bluish cast to the tongue.
The best way to diagnose the condition is with an endoscope, which usually means going to an internal medicine specialist, but your own veterinarian may be able to take a series of radiographs (X-rays) to diagnose the condition. The trachea changes its dimensions as the dog breathes in and out, so a single radiograph often misses the critical time of change.
In severe cases, the best option may be implanted prosthetic supports. A specialist who has experience in this type of surgery must perform this procedure because it’s complex. The nature of the surgery means that it isn’t always successful.
Tip
In less-severe cases of tracheal collapse, the following adjustments may help:
– Reducing weight
– Using a harness rather than a collar
– Humidifying the air
– Avoiding irritants such as cigarette smoke
– Avoiding any situation that may lead to overheating, stress, heavy panting, or coughing
– Taking glucosamine and vitamin C supplements to strengthen cartilage
– Using bronchodilators (this practice is controversial)
Selecting a specialistJust as you see a specialist when your health problems are more complex than your family practitioner normally handles, your dog may also benefit from a veterinary specialist. Don’t be afraid to ask whether a specialist could help. Most veterinarians are pleased that you asked and will find the appropriate specialist, set up an appointment for you, and send along any medical records. A specialist can be expensive, so consider asking about fees before you go. The American Veterinary Medical Association presently recognizes 20 specialties. You can find specialists in your area by going to the Web sites of the appropriate specialty organization. The ones you’re more likely to need are – American College of Veterinary Behaviorists: www.dacvb.org
– American College of Veterinary Dermatology: www.acvd.org
– American College of Veterinary Internal Medicine: www.acvim.org
– American College of Veterinary Ophthalmologists: www.acvo.org
– American College of Veterinary Surgeons: www.acvs.org
– American Veterinary Dental College: www.avdc.org
|
Dealing with Emergencies
If you face an emergency with your Pom, remember to stay calm. Your calm voice is the best medicine at first.
Remember
If your dog appears to be severely injured, start with the ABCs of first aid (I explain them in this section). Then call your veterinarian or go to the emergency clinic — and drive carefully! What would happen to your sick dog if you had an accident and ended up going to the hospital yourself?
A is for airway
Small dogs can choke on dog treats, small balls, rawhide, bones, toys, and other items around the house and yard. A choking dog may paw frantically at his mouth, try to retch, or make heaving chest motions — but he can’t breathe.
Open his mouth and either pull his tongue forward or push down on the back of the tongue. Then look and gently feel for any obstructions. If you can see an obstruction, try to gently reach two fingers in and extract it. But if this doesn’t work, use the Heimlich maneuver.
1. Hold him against your chest, head up, and facing away from you.
2. Place your fist just beneath the end of his sternum (chest bone).
3. Grasp that fist with your other hand and give five rapid thrusts inward and upward.
4. Check the airway and repeat Steps 1 through 3 if needed.
5. If he’s unconscious, give artificial respiration (see the next section).
B is for breathing
Is he breathing? Is his chest rising and falling? If not, check for obstructions (see the previous section). If no obstruction is present, perform artificial resuscitation.
1. Place him down on his side.
2. Open the mouth, clear away any mucus, and pull the tongue forward. Seal your mouth over the dog’s nose and mouth.
3. Blow gently into the nose for two seconds, then release.
Use gentle puffs. Pomeranians have very small lungs. Blow just enough to see the chest rise. If the chest doesn’t rise, blow harder, make a tighter seal around the lips, or check again for an obstruction.
4. Repeat Step 3 at the rate of one breath every five seconds, stopping after one minute to monitor breathing and pulse.
5. Repeat Steps 3 and 4 until he’s breathing on his own.
6. When he does resume breathing, get him to the vet.
C is for circulation
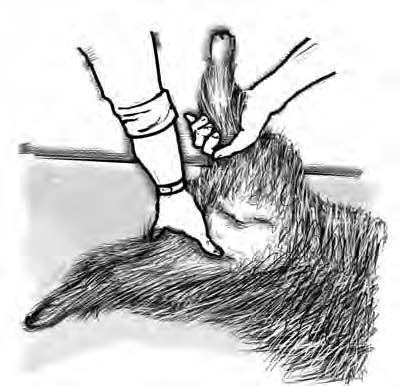
Check your dog’s pulse by placing your fingers on his femoral artery (inside the thigh, near where the rear leg meets the abdomen — see Figure 11-1) or on his left chest just behind the elbow. Also check the tongue and gum color. If they’re bluish or if the gums are pale, he’s not getting enough oxygen but may still be breathing. In this case, evaluate him for shock.
Figure 11-1: Where to take a Pom’s pulse.
If you’re sure his heart isn’t beating, begin cardiopulmonary resuscitation (CPR):
1. Place him on his right side on a table or floor.
2. Place your fingertips (one hand on top of the other) on his left chest about 1 inch up from and behind the elbow.
3. Press down and quickly release at the rate of one compression per second.
4. After every 10 to 15 compressions, stop to give two breaths through the nose (see the previous section). If you have a helper, you can continue while your helper gives breaths every 3 to 4 compressions.
5. Continue with Steps 2 through 4 until you feel a pulse. Then get him to the vet.
by D.Caroline Coile,Ph.D.